
MY JOURNEY WITH RHEUMATOID ARTHRITIS PART ONE
This post may contain affiliate links
Rheumatoid arthritis has changed my life and the journey is going to be long one ! This post has taking over a year to write. And this is my journey taking place in Essex during 2017 and 2018. This is the website that I have been using for research how to manage this condition
Why does it hurt so much?
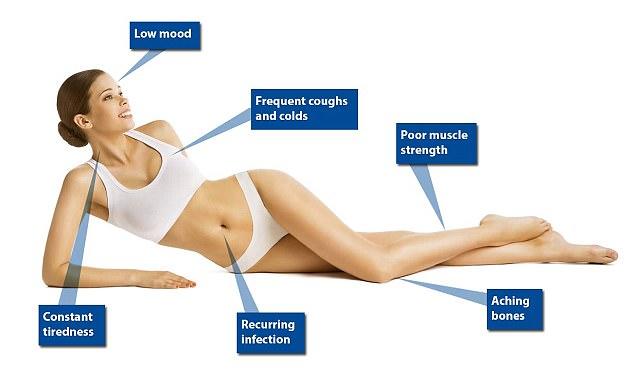
I have had painful arms and fingers for the last five years. They would ache and hurt so much and I could never work out why. And in addition, I was always picking up every bug going around the office and always feeling so tired all the time. Well it turns out this was the start of my journey with rheumatoid arthritis. I could never understand why I hurt so much. This is what I have been suffering with for such a long time
- Morning stiffness for more than an hour in my hands, knees, elbows, hips, feet, or ankles that lasts at least six weeks
- Joint swelling, tenderness or pain, and sometimes redness.
- Symptoms that appear symmetrically across the body and in multiple joints
- Chronic inflammation
- Fatigue
Tendonitis – misdiagnosed?
I eventually went back to the doctors in 2015, when the eight Nuromols I was taken a day no longer worked on the pain. I was prescribed some stronger pain relief and advised to consider trying private physiotherapy. For £40 a time, I was told that I had tendonitis and was having treatment that included manual therapy, soft tissue massage, electrotherapy and acupuncture. This was done on both wrists. And this was pretty painful each time. And this did work for a time. After six weeks of these, the pain died down and then you think you are cured. But you are not really. The pain comes back and back and back. And I had this in both arms within a nine month period in 2016.

Rheumatoid Arthritis Question?
So much so, that I had to book more appointments at the doctors and in early 2017 they signed me off work and just prescribed even stronger pain relief. And guess what, this new pain relief does not work either. And then finally, you see a doctor who looks at your records, sees your hands are swollen and painful and just listens to you. I was told to have lots of blood tests and eventually told I had a severe vitamin d deficiency and this was looking like it was going to be rheumatoid arthritis. So I was then prescribed
- Alendronic acid 70mg tablets – Bone protection
- Calceos 500mg/400unit – Calcium and Vitamin D Supplement
- Lansoprazole 15mg – Stomach protection
- Prednisolone 5mg – Steriods
- Fultium-D3 20,000unit capsules – seven week high dosage Vitamin D
Introduction To Prednisolone Steriod
Prednisolone was a stronger pain relief, I started taking 40mg daily as I was booked to go to China in three weeks and I was not sure that with this much pain I was able to go. I even went to this appointment with my mum, because sometimes you just need some support. Hallelujah, they worked – finally a pain relief that did what it said it would do. But it did bring over complications, I started with
- insomnia – I started sleeping for less than five hours a night
- gradual weight gain – mine is around my face and my husband does not like it
- weaker immune system – I did pick up a few colds from visitors
But a good thing other than feeling better, was I did not suffer from the bad hay fever than the UK had that summer. I remember my best friend really suffering with it. And my periods stopped completely.

Private Treatment In The UK And The Introduction Of DMARD’s
Now when I was told that I had I was being referred to my local hospital to see what was happening with my arms and hands. I had to wait a long time. I was referred in April but was told that there was a lot of problems in the local hospital with rheumatologist doctors leaving and lots of changes within the department. My appointment came through for late July. I had forgot that I had a private medical programme. So the next time, I had a doctors appointment in late May, I asked him and he told me that it might be the way to be seen earlier. And this was true, I got an appointment within a week. I meet a rheumatologist doctor in early June who told me at length about the dangers of steriods and that I should come off them. He examined me and agreed with my doctor with the diagnosis of rheumatoid arthritis. He then prescribed Hydroxychloroquine a 200 mg dose, which I take daily. This new medication would take over three months to work. Another appointment and an xray revealed that I had periarticular osteopenia and sero-negative rheumatoid arthritis. I was then prescribed Methotrexate a 15 mg that I take weekly. Both these new drugs are DMARDS, which are disease-modifying anti-rheumatic drugs. They work by blocking the effects of the chemicals released when the immune system attacks the joints, which could otherwise cause further damage to nearby bones, tendons, ligaments and cartilage. They also take over three months to actually work. So for me this was August bank holiday, I was hoping to feel so much better. He also told me that I should not be paying out with my private medical programme for this and he referred me back to my local hospital.
Daily Struggles
The first rheumatologist told me back in June, that you can live a normal life with this disease. But in my case, I have not been normal since November, nearly a year before and still not on the right medication. Each day it is horrible, waking up with stiffness, aching and painful joints. And what does not help, that if you worry and get stressed about your situation, this only makes it worse. But also for me, I hate needles, so having monthly blood tests and then steroid injections and a flu jab. This has all taking a toll on me.
Steroid Withdrawal
You can not go cold turkey with steriods, you have to reduce them by tapering them. Every week, I had reduce them down by 1 tablet, 1 less 5mg. Now I did not have a problem with this. But did not expect to then experience fatigue every day and sleeping every afternoon for between ninety minutes and three hours. And then still sleeping eight to nine hours the same night. My doctor told me this was completely normal for steroid withdrawal. But I continued until I was off and then within days I had what I now know are flare ups. Imagine walking up at 4.30am in the morning in pain, not being able to get back to sleep until you do eventually pass out. And then you have painful arms and hands until you pass out again the same day and that is what happened. So again back to the doctor, who advised that although it was good to come off the steriods. Due to appearance of the hands, and my latest blood test which had revealed that my inflammation levels had rised. He told me to go back onto the steriods. And then suggested, the next time I go to the hospital, he would write to them requesting that I go onto the next stage of treatment, as I have an aggressive case. Now this scared me, as when looking it up, it would involved either a weekly, fortnightly or monthly injection. Or a monthly iv, or self medication with like an epi pen once you have had training. Luckily for me, my appointment came through within the week. But by the end of August, the DMARD’s were having no effect on me at all.
Rheumatology At Local Hospital
At the hospital, my new rheumatologist told me she was disappointed that I was back on the steroids. She wants to see me when I am at my worst. But it is not as if I can press a button. Photos only show so much. My blood work which can only been taking during the week at the moment, is masked by both my steroid injections and oral steroids. So I am back to reducing my steroids and being in pain and hopefully I can live with the pain in time for my next appointment at the Rheumatology clinic. So a month later in September, I was back at the hospital, still not clear of the steroids as the injections last for eight weeks. My inflammation levels are still high, so my Methotrexate was increased to 20 mg for another eight weeks. I now have to wait for the steroids to get out of my system, and then to have a ultrasound to see all the inflammation.
The Drugs Do Not Work
But during this eight week wait, more inflammation flared up in my knees. Leaving me house bound and have daily hot baths to soothe all my painful joints. So much that my mum suggested it was maybe time to get a walking stick. Now this shocked me, so I telephoned the hospital asking when my appointment for my ultrasound was, this about four weeks in. And to my shock, I found out that it was not even booked in. My rheumatologist had forget to refer me. But before the ultrasound, I suffered more flare ups. Which left me in agony and I had so much pain in lots of joints and was very emotional daily. And my doctor in late October said that I could go back to my private plan but my long term care would still be under the NHS. And he would contact the hospital again now that he has seen the state of me. And he also informed that the next treatment would take another six to eight weeks to work. This is going to be a nightmare, which this year has been for me so far. At the end of October, I got my dates for a clinical nurse appointment – 30th November 2017 and my next appointment with the rheumatologist was the 3rd January 2018. And due to the pain, I was in, I promptly contacted my local doctors and asked them to refer back to a private hospital just to be seen earlier.

Back On Private Treatment
You have to remember I am been in pain since November of 2016 and signed off work since February 2017. And I got an appointment within a week. This annoys me, why can the NHS work like this. We pay out a lot of money from our payslips in tax and national insurance why can we not have a state of the art 24 hour health service. And this all comes down to money. I used to get private healthcare with my employers but lost this in 2011. But I started a private plan in 2009 and for me this year it has literally been so useful to be seen early every time. And I was booked in with the same private rheumatologist who I saw in June. He examined me, commented on how much I had changed and discussed at length what we could do. It turns out that as I am having no relief from the current rheumatoid arthritis medication. And he also noted that I will more than likely have to have knee surgery in the future. And he could see this just by looking at my legs. I am now booked in for an MRI on my hands, my insurance only goes so far. And thankfully, he has now prescribed a new drug called Etoricoxib – another DMARDS which should work just like the steriods but not do the damage that they do. So fingers crossed, he said in a few days I would started to feel better. Lets hope so ! And I feel just a 40 mins appointment I processed further than the last three months under the NHS. Which is such a shame. I am pleased to say that these new pills do work on my hands. But not my knees. And I contacted the Patient Advise & Liaison Services (PALS) as I not getting anywhere with my NHS treatment. And I still have not been booked in for my ultrasound. And then the same day I get the results from my MRI, I get call from PALS to say that the appointments booked are a mistake. I am due to see the rheumatologist at the end of November, two months earlier than I was told. I have to thank my friend Tasha who told me to contact PALS, I never knew anything about them.

My MRI confirmed the inflammation and that it an auto immune arthritis. We have increased the Etorcoxib to the maxim of 90 mg. This until I see the rheumatologist on the NHS and move onto the biological treatments. The more expensive drugs which are not easy to get.
Back With The NHS
So back to my local NHS in Essex and I had a ultra sound on my fingers. Even though I told the medical personnel that it is my wrists, elbow and knees that are painful. This ultrasound showed no inflammation. And the next appointment, with the rheumatologist made my decision easy. She confirmed after seeing my MRI scan (done at the private hospital) that I had inflammation and my levels of inflammation in my blood tests also proved this. She also kept insisting that the MRI showed I had trauma to my left wrist. I have never had trauma (broken bones, accidental.) So that was concerning as you know what happens with your own body. She also asked me to pick between her and my private doctor. And could not understand why I was seeing him. Also she was totally ambivalent about the care I had received in this clinic. I am so pleased that I had already asked my doctor to refer me back to my private rheumatologist who works for the NHS in Cambridge. I asked him in November, what he would prescribed if he was my NHS doctor. He told me them he would put me on the biological treatments and invited me to see him in Cambridge. I only live one hour drive away and my mum who has gone to most of the hospital both NHS and private agreed with me. I only wished that I had known I could have done this sooner. But the very next day I got a call from my local NHS hospital in Essex, offering me an appointment to do the biological test the very next week. I agreed as I want this sorted sooner rather than later.
Biological Treatments
My best friend was already on a biological treatment called humira due to having crohn’s disease. I have been told to ask for this, but you can not get this easily. In Essex, as it more expensive, you have to prove that the toxic pills you take daily are not working. And my monthly blood tests when I was finally free on steroids in early October proved this. However, there is still a test that you have to go through with a nurse. This for me took place in another hospital within Mid Essex. The test with a nurse involved lots of questions and examining the joints. The nurse confirmed that I should qualify for humira. The request for the funding was put through to the Mid Essex Clinical Commissioning Group (CCG) and I should hear within twelve weeks. And to my surprise I got a phone call within ten days to confirm that I have been approved. To say that I was over the moon was a understatement. I just hope that this works for me on a long term basis and does not do a lot of damage to my internal organs.

My biological treatment arrived in January from a company called Healthcare At Home. I am a bit nervous about self injecting. It is because I have such a hatred of needles and injections overall. And I can not stop myself worrying about every blood test I have this past twelve months. My local GP knows this and just springs them on me. I am much likely to agree on the spot and get it done. Then have a booked appointment and have to think and worry about it. I have to self inject every two weeks.
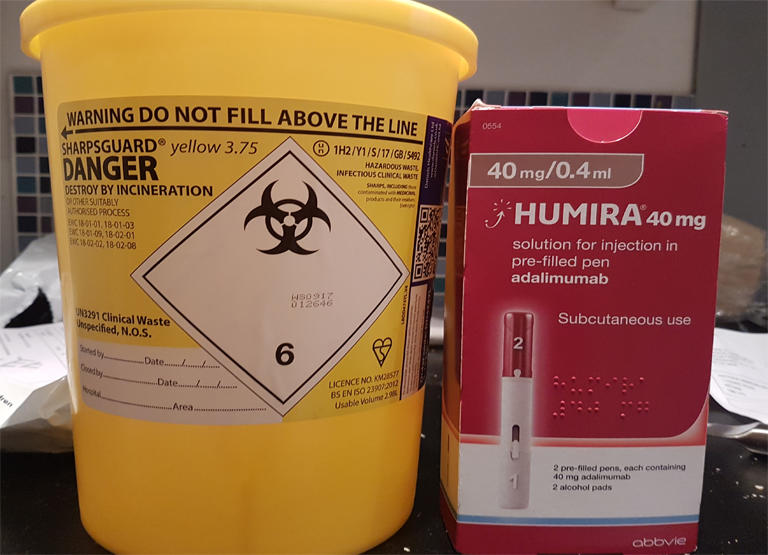

And my first appointment with Health At Home was cancelled on the same day, as there was no nurse available. Why book someone an appointment, if there is no nurse available, and then call on that same day. I am not impressed with this part of the NHS either so far. And now have to wait for a phone call for another appointment. The nurse from Health At Home had come to Essex all the way from South London. He was really nice and talked at length about the process and then I self injected. So lets hope in the next two to twelve weeks that this new medication works. A week after the injection, I woke up with no stiffness and this was nice. And I was not tired. I know I have to sleep for eight hours. And that same day, I was not tired. This has been a big change for me and I was pleased. But the pain in the arms, knees and now hip is still there. So lets see what happens.
.
Back at new hospital, my next NHS appointment, now I am under my (private) rheumatologist in Newmarket. And when you change hospitals during treatment. Even though you have already seen the doctor privately, you are registered as a new patient. And that meant, blood tests and x rays and this was unfortunate for me. But the staff there who took my tests were so nice. And I really liked this hospital. My husband said it is like a very old hospital. However, inflammation two days before the appointment flared up in one of my hips. All I can think is when is this going to stop ! Back again in three months, when hopefully the new drugs have had three months to work !
Winter 2018 & Lower Immune System
What I am still struggling with is my immune system. Whenever I went to the doctors I would pick up germs. And that is what I have to remember if I am unlucky to pick up something it will take at least two weeks to work through my body. This is something that I need to get under control. It was Christmas Day in 2017, that I started to get ill. So much that from Boxing Day until the second week in February of 2018. I had various fevers, diarrhoea, vomiting, all things that were very unpleasant. And even when the bugs passed I was still in pain and I think that it is the cold winter. I think UK winters are going to effect me every year. Now I need to plan around that and think how to avoid this situation.
Travelling
How during this time, I was signed off, I did travel to China, Slovenia, Germany, Spain, Italy, France and Malta. But I had complications. In China, I only slept for three to four hours a night and struggled every day with pain and tiredness. Not ideal when you are on a holiday of your lifetime, somewhere you have been dreaming off for years. In Slovenia, by this time, I was reducing my steriods, so by lunchtime every day, my fingers swelled and my fatigue kicked in. What was good for me, was that my husband could see the differences in me. I had booked two full day tours and one half day tour and it was pretty evident that this was too much for me. Germany was a mistake as both my husband having broken ribs and me in my poor health should not have gone too. And we both spend a lot of time resting and sleeping. Spain was my last weekend trip ever. We did not see much and only had a one full day tour but even then that was too much. Once I was home, I then spent the next two days sleeping over twelve hours to recover. I then went to Rome for four nights, I only booked two half day tours. This was a test to see if taking a city in slowly was do-able. And it was not. I had booked 2 half day tours, but every day like in Slovenia, my body gave up. I would have to return to the hotel and sleep for between ninety minutes and two hours. And my legs hurt so much. So it does look like that city breaks are going to be a no go unless my medication has changed for the better. We were supposed to go to Cape Verde in the winter, but we decided to cancel this as I was not in a good way. And I went to France with my friend. But again by lunchtime, my body would give up. So I would again return to our hotel to rest and sleep. It was disappointing but there was nothing I could do. And my friend knew this before we went away. The following year, after two months of being on Humira, my mum and I decided to go to Malta, to test out if I could handle travelling again. But with the knees still in pain, I can only manage to explore either in the morning or afternoon. And I also need to spend a day resting, as the actual travelling – plane journey and everything else involved really wears me out. It is not going to stop me travelling. This is passion of mine, and I just need to be mindful and take my time.
Thank you for reading if you got to the end of this post. I do intend to write another post about my continued experiences.






No Comments